Overview
Blood pressure and kidney health are deeply interconnected. This relationship plays a pivotal role in the overall functioning of the body. While the kidneys are essential for filtering waste and maintaining fluid balance, blood pressure ensures that this process is carried out efficiently. Disruption in either can create a cycle of complications, impacting an individual’s health significantly.
Understanding Blood Pressure and Kidney Function
Blood pressure refers to the force exerted by circulating blood on the walls of arteries. Healthy kidneys rely on consistent blood flow to filter and remove waste products and excess fluids. The filtration process is managed by nephrons, tiny structures in the kidneys that depend on an adequate blood supply.
When blood pressure rises or falls beyond normal levels, the kidneys are directly affected. High blood pressure, or hypertension, can damage the blood vessels in the kidneys, reducing their ability to function properly. Conversely, poorly functioning kidneys can lead to fluid retention, which can elevate blood pressure further.
The Effects of High Blood Pressure on Kidneys
Hypertension is one of the leading causes of kidney disease. Over time, consistently high blood pressure can lead to narrowing or weakening of the arteries in the kidneys. This reduces the kidneys’ efficiency, causing waste products to build up in the bloodstream.
Chronic kidney disease (CKD) often results from prolonged high blood pressure. CKD is a condition where kidney function declines over time, which can progress to kidney failure if left untreated. In severe cases, dialysis or a kidney transplant becomes necessary to sustain life.
The Role of the Kidneys in Regulating Blood Pressure
The kidneys are not just passive recipients in this relationship. They actively regulate blood pressure through a hormone system called the renin-angiotensin-aldosterone system (RAAS). When blood pressure drops, the kidneys release renin, an enzyme that triggers a chain of reactions to raise blood pressure and restore balance.
This system ensures that the body maintains the right level of sodium and water, which are crucial for blood pressure stability. However, when the kidneys are damaged or overburdened, this regulatory mechanism may malfunction, causing blood pressure to remain consistently high.
Symptoms of Kidney Problems Related to Blood Pressure
Kidney issues linked to abnormal blood pressure often progress silently. Symptoms may only appear in advanced stages, making regular health checks essential. Common signs include:
- Swelling in the legs, ankles, or face: This may occur due to fluid retention caused by poor kidney function.
- Changes in urination patterns: Reduced output, foamy urine, or the presence of blood in the urine can indicate kidney stress.
- Fatigue and weakness: A buildup of toxins in the body due to impaired kidney function can cause persistent tiredness.
- Shortness of breath: Fluid retention can lead to congestion in the lungs, making it hard to breathe.
- High blood pressure readings: This is often the first detectable sign that the kidneys are struggling.
Managing the Relationship Between Blood Pressure and Kidney Health
Preventing damage to the kidneys requires a proactive approach to maintaining healthy blood pressure levels. This involves adopting a combination of lifestyle changes, medical treatments, and regular monitoring.
Dietary Choices
A balanced diet low in salt and rich in fruits, vegetables, and whole grains supports both blood pressure and kidney health. Reducing sodium intake helps prevent fluid retention and lessens the strain on the kidneys.
Physical Activity
Regular exercise strengthens the heart and blood vessels, aiding in the regulation of blood pressure. Moderate activities such as walking, cycling, or swimming are beneficial and reduce the risk of hypertension.
Adequate Hydration
Staying hydrated supports kidney function by aiding in the removal of waste products. Drinking water in recommended amounts is essential, but excessive fluid intake should be avoided in cases of existing kidney damage.
Medical Management
For individuals with hypertension or kidney disease, prescribed medications such as ACE inhibitors or angiotensin receptor blockers (ARBs) help manage blood pressure and protect kidney function. Regular consultations with healthcare providers ensure proper adjustments to treatment plans.
Avoiding Harmful Substances
Smoking, excessive alcohol consumption, and certain over-the-counter medications can exacerbate kidney problems and increase blood pressure. Avoiding these substances reduces the risk of complications.
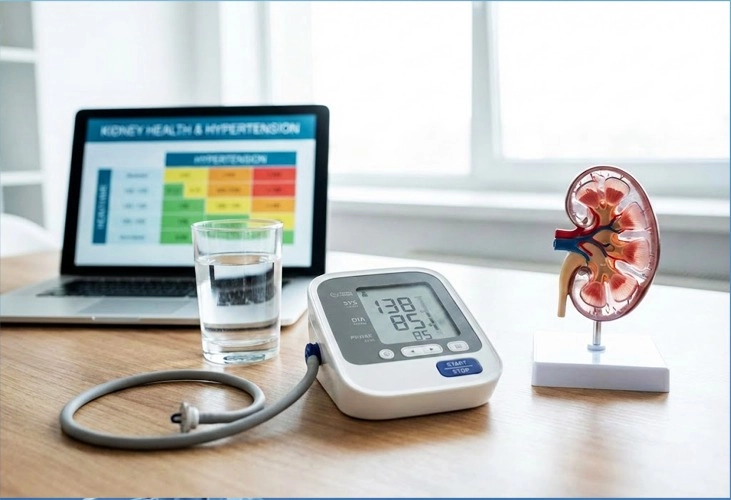
Monitoring Blood Pressure and Kidney Function
Regular checkups help detect abnormalities early. Blood pressure readings and simple urine and blood tests can provide insights into kidney health and guide preventive measures.
The Impact of High Blood Pressure on Kidney Disease Progression
For those already diagnosed with chronic kidney disease, uncontrolled high blood pressure accelerates the loss of kidney function. Careful blood pressure management can slow this progression and delay the need for more intensive treatments such as dialysis.
Similarly, people with hypertension should remain vigilant for any signs of kidney involvement. Early intervention minimizes the long-term impact on both organs.
Raising Awareness About the Connection
Educating individuals about the link between blood pressure and kidney health is crucial. Many people remain unaware of how closely these systems interact and the potential risks posed by neglecting one or the other.
Communities, healthcare providers, and organizations can play a role by encouraging regular health screenings, promoting healthy lifestyles, and making information accessible.
Conclusion
Blood pressure and kidney health are intricately connected, each influencing the other in profound ways. Maintaining healthy blood pressure levels is essential for preserving kidney function while ensuring kidney health contributes to stable blood pressure.
Proactive care, including lifestyle changes and medical oversight, is key to breaking the cycle of damage that can arise from neglecting these aspects of health. With early intervention and consistent monitoring, individuals can significantly reduce their risk of complications, supporting both kidney function and overall well-being.